Diagnosing Atrial Fibrillation: Understanding the Testing Process

Diagnosing Atrial Fibrillation (AFib) can be a complex process that requires a good understanding of the testing involved. Understanding the testing process is crucial in accurately diagnosing atrial fibrillation and developing an effective treatment plan.
What Is Atrial Fibrillation and How Is It Diagnosed?
Atrial fibrillation is a condition characterized by irregular and often rapid heart rate, resulting in poor blood flow and potential complications such as heart failure and stroke. It is often diagnosed through an electrocardiogram (ECG) which measures the electrical activity of the heart and can detect irregularities in the heart's rhythm. Other diagnostic methods may include a Holter monitor to monitor heart rhythms over some time, and blood tests to check for underlying causes such as thyroid issues or heart damage.
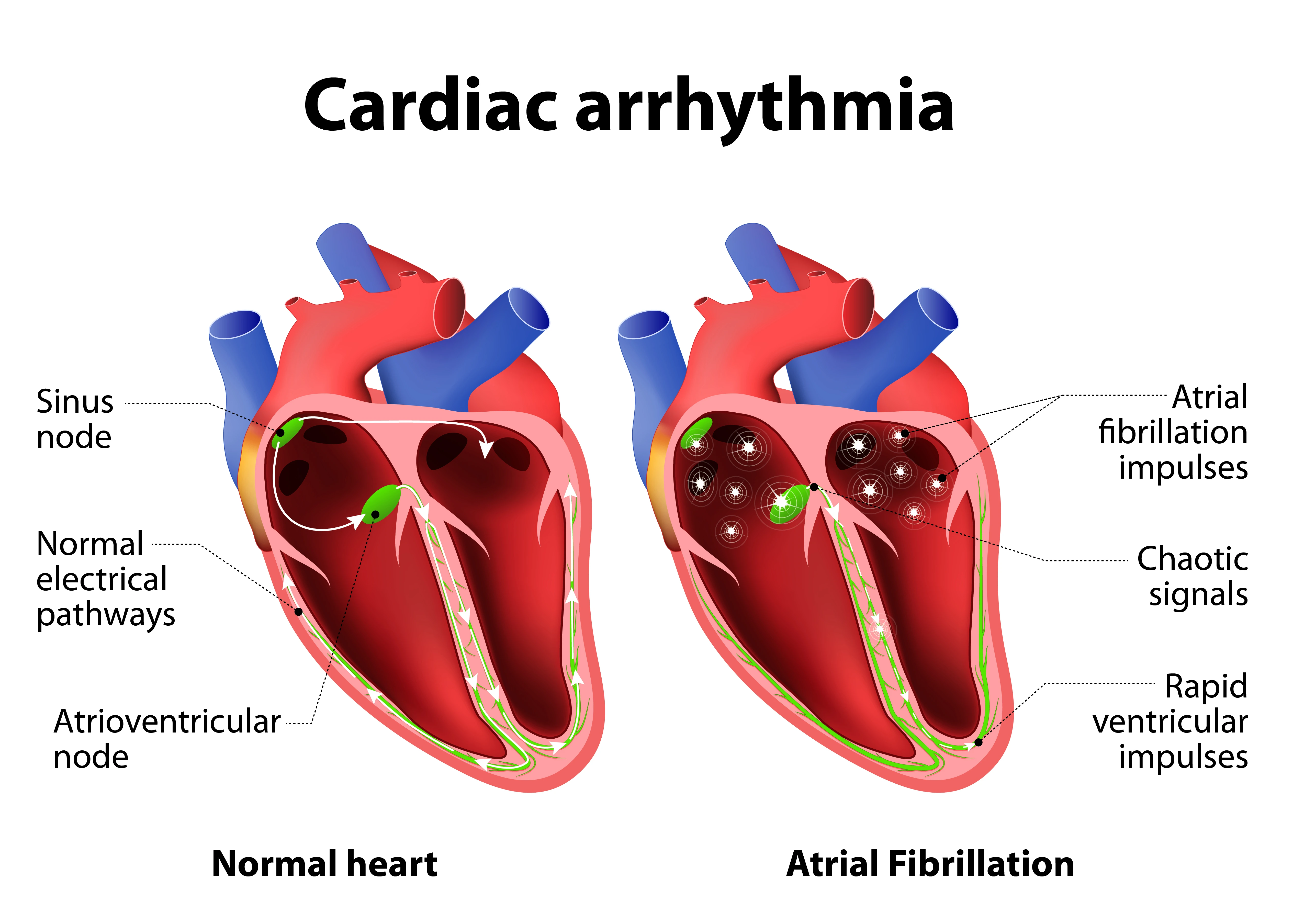
Understanding Atrial Fibrillation and Its Impact on Heart Rhythm
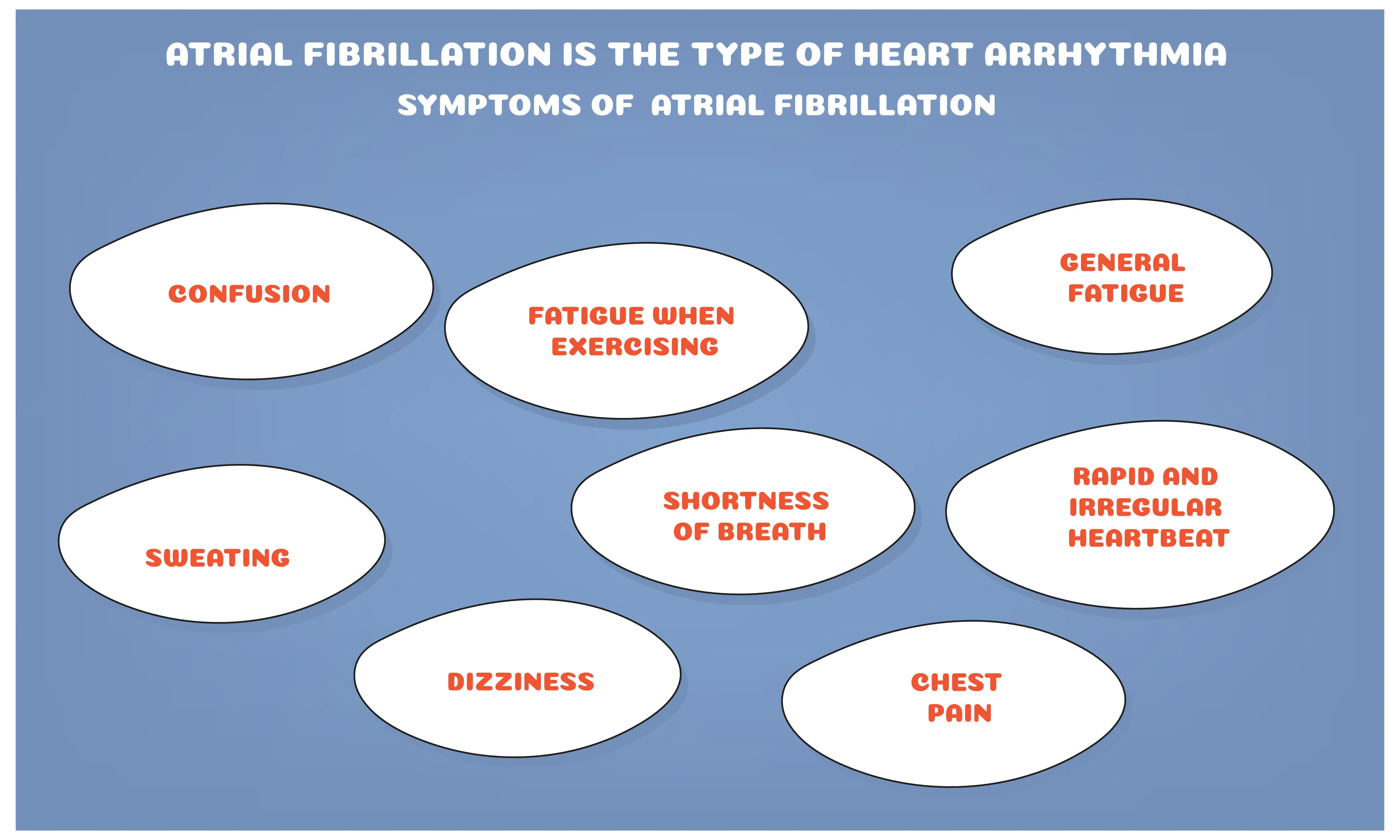
AFib is a heart condition where the upper chambers of the heart beat irregularly, causing an erratic heart rhythm. This can lead to symptoms such as palpitations, dizziness, and shortness of breath. It can also increase the risk of stroke and heart failure. Understanding the impact of atrial fibrillation on heart rhythm is crucial in managing the condition and preventing further complications.
Electrocardiogram (ECG) and Its Role in Diagnosing Atrial Fibrillation
The Electrocardiogram (ECG) measures the electrical activity of the heart and can detect abnormal heartbeats, such as those characteristic of Atrial Fibrillation. By analysing the patterns and timing of the electrical signals, Cardiologists can accurately diagnose Atrial Fibrillation and develop appropriate treatment plans for patients.
Diagnostic Blood Tests for Detecting Atrial Fibrillation
Diagnostic blood tests can measure levels of specific markers in the blood that may indicate AFib. By detecting these markers, a cardiology doctor can diagnose and treat them early, reducing the risk of complications and improving patient outcomes.
Significance of Holter Monitoring in Identifying Atrial Fibrillation
Holter monitoring plays a significant role in identifying AFib. By continuously recording the heart's electrical activity for 24-48 hours, it can detect intermittent episodes of atrial fibrillation that may go unnoticed during a regular ECG. This allows for more accurate diagnosis and appropriate management of the condition.
Echocardiogram: Using Sound Waves to Assess Atrial Fibrillation
An echocardiogram is a non-invasive procedure that uses sound waves to create a moving picture of the heart. By using sound waves to visualise the heart's structure and function, heart doctors can diagnose and monitor atrial fibrillation more effectively.
What Are the Symptoms of Atrial Fibrillation and How Are They Tested?
The symptoms of Atrial Fibrillation include palpitations, shortness of breath, weakness, dizziness, chest pain, and fatigue. To test for Atrial Fibrillation, a doctor may conduct an ECG or a 24-hour Holter Monitor. Other tests may include a stress test, echocardiogram, or blood tests to check for underlying causes such as thyroid problems or heart disease.
Recognising Irregular Heart Rate as a Symptom of Atrial Fibrillation
Recognising irregular heart rate as a symptom of atrial fibrillation is crucial for early detection and management of the condition as it can lead to potential complications such as blood clots and stroke. Monitoring heart rate and seeking medical advice if irregularities are observed can be critical in preventing serious health consequences.
Blood Tests for Detecting Heart Failure and Assessing Atrial Fibrillation
Blood tests are crucial for detecting heart failure and assessing atrial fibrillation. For heart failure, blood tests can measure levels of certain proteins and substances that indicate the heart's condition, such as B-type natriuretic peptide (BNP) and troponin. In the case of atrial fibrillation, blood tests can detect markers of clotting and inflammation, helping to assess the risk of stroke.
Assessing the Electrical Activity of the Heart Through ECG
By placing electrodes on the skin, the ECG machine can measure the electrical impulses as they travel through the heart. This allows healthcare professionals to identify any irregularities or abnormalities in the heart's electrical system and to make informed decisions about treatment and care.
Understanding the Role of Stress Tests in Detecting Atrial Fibrillation
By subjecting the heart to physical exertion through targeted physical activity, stress tests can uncover irregular heart rhythms that may not be present at rest. This is especially important since atrial fibrillation can often be asymptomatic. Stress tests can help physicians identify potential arrhythmias and determine the best course of treatment for their patients.
Different Diagnostic Tests and Procedures Used to Identify Atrial Fibrillation
There are several different tests and procedures that can be used to diagnose AFib. These may include an electrocardiogram (ECG), a Holter monitor, a cardiac event recorder, an implantable loop recorder (ILR), an echocardiogram, a stress test, or blood tests to check for thyroid function and other underlying conditions. In some cases, a doctor may also recommend a procedure called an electrophysiology study, which involves threading thin, flexible tubes (catheters) with electrodes through blood vessels to the heart to test its electrical activity and identify the source of the arrhythmia.
What Are the Risks and Complications Associated with Atrial Fibrillation Testing?
Atrial Fibrillation testing carries certain risks and potential complications. There is a small risk of bleeding or bruising at the site where the blood sample is taken. Additionally, some people may experience lightheadedness or fainting during the testing procedure. In rare cases, the test may cause a blood clot to form, leading to potential blockage of the blood vessels. It is important for individuals undergoing Atrial Fibrillation testing to be aware of these potential risks and to report any unusual symptoms to their Cardiologist.
Assessing the Risk of Blood Clots in Patients with Atrial Fibrillation
Atrial fibrillation increases the risk of blood clots forming in the heart, which can travel to the brain and cause a stroke. Physicians use scoring systems, such as the CHA2DS2-VASc (a point-based system used to stratify the risk of stroke), to assess this risk and make informed decisions about anticoagulant therapy for their patients.
| CHA2DS2-VASc risk | Score |
|---|---|
| Age ⥸75 | 2 |
| Stroke/TIA/Thromboembolism | 2 |
| Hypertension | 1 |
| Diabetes | 1 |
| Vascular Disease | 1 |
| Age 65-74 | 1 |
| Female | 1 |
Understanding Abnormal Heart Rhythms and Their Impact on Health
Abnormal heart rhythms, also known as arrhythmias, can lead to complications such as blood clots, stroke, heart failure, and other cardiovascular issues. Understanding the underlying causes and effects of abnormal heart rhythms is crucial for proper diagnosis and treatment to ensure better heart health.
Assessing the Role of Atrial Fibrillation Testing in Identifying Heart Valve Issues
By monitoring irregular heart rhythms, a cardiologist can promptly detect any potential valve problems. This is because heart valves are responsible for opening and closing to allow blood to flow through the heart in the correct direction. When a valve is damaged or malfunctioning, it can cause irregular heartbeats, which can be a sign of an underlying valve problem.
Recognizing the Importance of Regular Physical Exams in Atrial Fibrillation Detection
Early detection through physical exams, including a screen for atrial fibrillation, can lead to proper management and treatment, reducing the risk of stroke and heart failure. The management of atrial fibrillation is crucial as early detection allows for interventions to be put in place before the condition worsens. It is best to take proactive steps towards maintaining their heart health and overall well-being.
Evaluating the Impact of Family History on Atrial Fibrillation Diagnosis
Research has shown that individuals with a family history of atrial fibrillation are at a higher risk of developing the condition themselves. Evaluating family history as a potential factor can aid in early detection and intervention.
Assessing the Importance of Regular Heart Rate and Rhythm Monitoring in Atrial Fibrillation
Monitoring the heart rhythm and rate allows cardiology doctors to assess the effectiveness of medications, identify potential complications, and make informed decisions about treatment options. This ongoing monitoring is essential for maintaining heart health and minimising the risk of complications.
Frequently Asked Questions About Atrial Fibrillation Testing
Atrial fibrillation testing is commonly done through an electrocardiogram (ECG) or a Holter monitor. Patients may wonder about the accuracy of these tests, the potential side effects, and the duration of the testing process. Fortunately, these and other common questions are addressed in a FAQ resource provided by healthcare professionals.
What Tests Are Done for Atrial Fibrillation?
The tests done may include an electrocardiogram (ECG), an ambulatory ECG heart monitor, an echocardiogram, and blood tests.
What Is the General Examination for Atrial Fibrillation?
The general examination for atrial fibrillation includes assessing the patient's heart rate, rhythm, and blood pressure. The doctor will also check for any physical signs of heart complications. Additionally, a medical history will be taken to identify any risk factors for atrial fibrillation, such as high blood pressure, diabetes, or heart disease.
Does Atrial Fibrillation Always Show Up on ECG?
Atrial fibrillation does not always show up on an ECG. This is because an ECG is a snapshot in time and atrial fibrillation can be intermittent (paroxysmal AF).
Can You Tell Atrial Fibrillation From Pulse?
In atrial fibrillation, the pulse is often irregular and can feel rapid or fluttery. By comparing the pulse to a regular rhythm and rate, heart doctors can often discern if a person may be experiencing atrial fibrillation.
Can You See AFib on a Pulse Oximeter?
Yes, AFib can sometimes be detected on a pulse oximeter. While a pulse oximeter primarily measures oxygen saturation in the blood, irregular heart rhythms like AFib can affect the readings. This is because AFib can cause the blood flow to pulsate irregularly, which can be picked up by the pulse oximeter's sensors.
How Can I Test for Atrial Fibrillation at Home?
There are a few ways to test for atrial fibrillation at home. One option is to use a handheld ECG device, such as a smartphone-based monitor, to record your heart's electrical activity.