Cardiac Tamponade: Causes, Symptoms, Diagnosis, and Treatment


Introduction
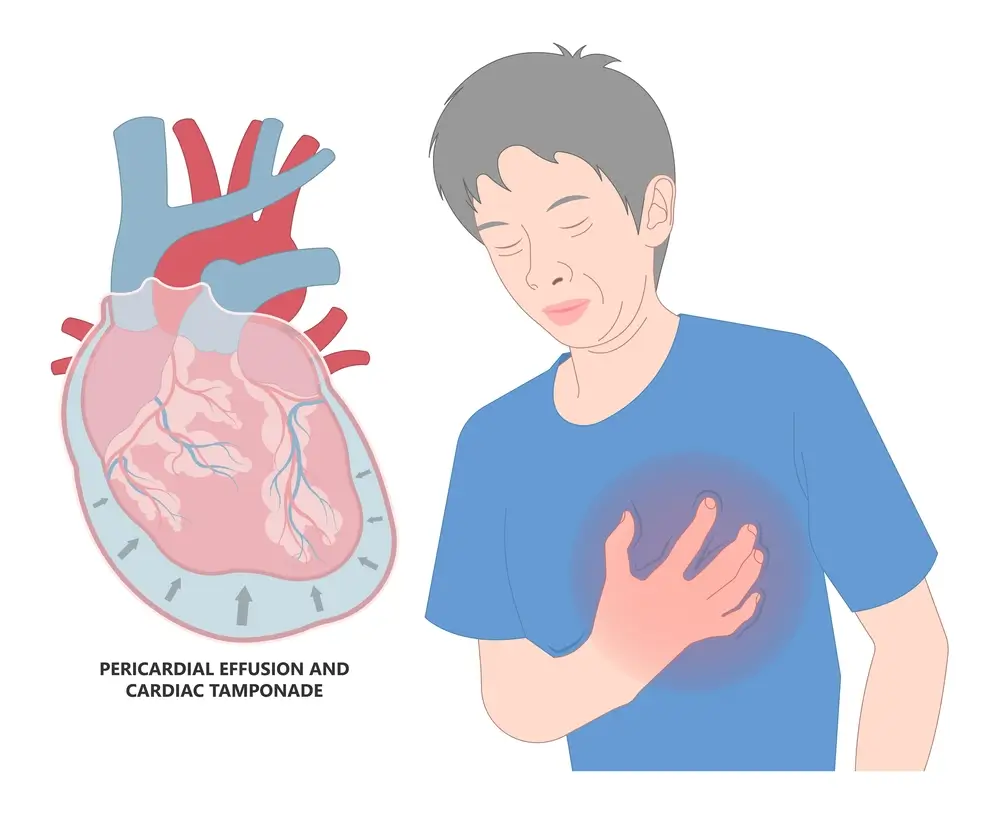
Cardiac tamponade is a life-threatening medical emergency that requires rapid diagnosis and intervention. It occurs when fluid accumulates in the pericardial sac—the thin, double-layered membrane surrounding the heart—leading to increased pressure and impaired cardiac function. This pressure restricts the heart’s ability to pump blood effectively, which can rapidly deteriorate into circulatory collapse if not treated immediately.
What is Cardiac Tamponade?
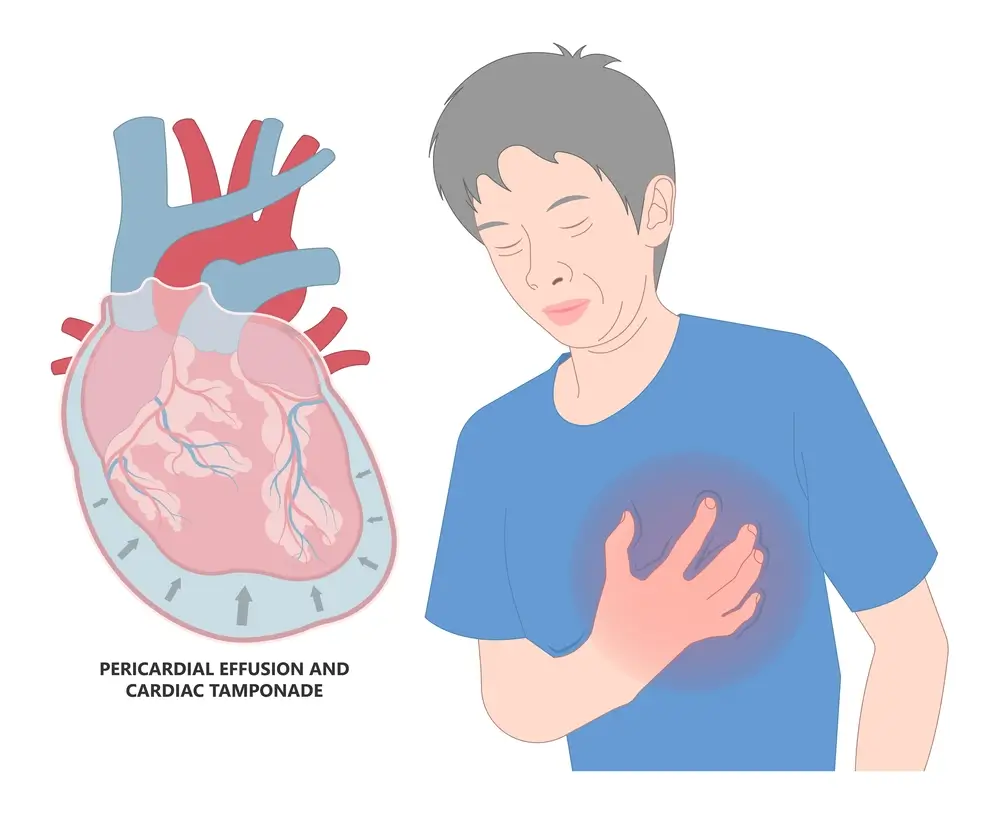
Cardiac tamponade is a condition in which fluid—often blood or exudate—accumulates rapidly or in large amounts in the pericardial space. This buildup exerts pressure on the heart, compressing the atria and ventricles, and impairing the heart's ability to fill and eject blood. The severity of tamponade depends not only on the volume of fluid but also on how quickly it accumulates.
Even a small amount of fluid can cause tamponade if it accumulates rapidly, whereas a slow buildup may not produce symptoms until the volume is significantly larger.
Types of Cardiac Tamponade
Understanding the forms of cardiac tamponade is essential in clinical assessment and management.
Acute Cardiac Tamponade
Occurs suddenly and is often caused by trauma, cardiac rupture, or a complication of invasive procedures. It is a medical emergency requiring immediate intervention.
Subacute Cardiac Tamponade
Develops more slowly over days or weeks. It may be caused by malignancy, uremia, or infection.
Chronic Cardiac Tamponade
This form develops over a long period and is usually due to chronic inflammation or cancer. It often presents with less dramatic but persistent symptoms.
Causes and Risk Factors
Identifying the underlying cause of cardiac tamponade is crucial for targeted treatment and preventing recurrence. The condition can result from a variety of cardiac and systemic issues.
Traumatic Causes
- Penetrating chest injuries (e.g., stab wounds)
- Blunt chest trauma (e.g., motor vehicle accidents)
- Complications from pacemaker or catheter insertion
Medical and Surgical Causes
- Post-cardiac surgery (post-pericardiotomy syndrome)
- Cardiac perforation during catheterisation or angioplasty
- Pericardial effusion post-myocardial infarction
Non-Traumatic Causes
- Malignancy (especially lung, breast, and hematologic cancers)
- Infections (e.g., tuberculosis, viral pericarditis)
- Autoimmune diseases (e.g., lupus, rheumatoid arthritis)
- Kidney failure (uremic pericarditis)
- Hypothyroidism
Patients with a history of pericardial disease, cancer, or chronic kidney disease are at higher risk. Visit our Heart Diseases page for more information on related cardiovascular concerns.
Symptoms of Cardiac Tamponade
Recognising the signs and symptoms of cardiac tamponade can save lives. The presentation varies based on the speed of fluid accumulation and the underlying cause.
Common Symptoms
- Chest pain or discomfort, often relieved by sitting up
- Shortness of breath (dyspnea), especially when lying flat
- Fatigue or weakness
- Palpitations
- Lightheadedness or fainting (syncope)
Physical Examination Findings
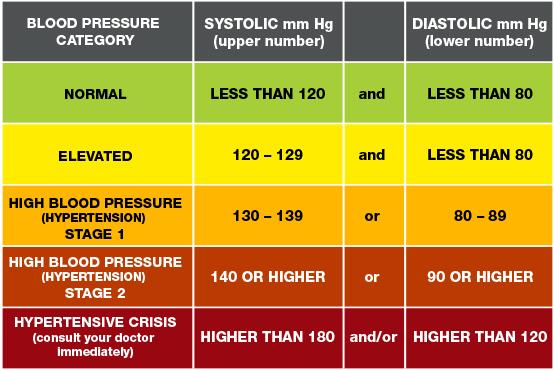
- Hypotension (low blood pressure)
- Jugular venous distention (JVD)
- Muffled or distant heart sounds
- Pulsus paradoxus (drop in blood pressure during inhalation)
- Tachycardia (elevated heart rate)
How Cardiac Tamponade Affects the Heart
To understand why cardiac tamponade is so dangerous, it helps to consider the heart's physiology. The pericardial sac normally contains a small amount of lubricating fluid (15–50 mL). In tamponade, rapid or excessive accumulation of fluid compresses the heart, particularly the right atrium and ventricle, reducing preload and impairing cardiac output.
This leads to:
- Decreased stroke volume and cardiac output
- Compensatory tachycardia
- Systemic hypotension
- Organ hypoperfusion
If untreated, cardiac tamponade can quickly progress to cardiogenic shock and death.
Diagnosis of Cardiac Tamponade
A timely and accurate diagnosis is vital for initiating life-saving interventions. Multiple diagnostic tools are used in combination to confirm tamponade.
Clinical Evaluation
- Observation of classic symptoms and signs
- Evaluation of medical history (e.g., cancer, recent procedures)
Electrocardiogram (ECG)
- Low-voltage QRS complexes
- Electrical alternans (varying QRS amplitude)
Chest X-Ray
- May show an enlarged, “water bottle”-shaped cardiac silhouette
- Less useful in early tamponade
Echocardiography (Echo)
The gold standard for diagnosis:
- Pericardial effusion
- Diastolic collapse of the right atrium or the right ventricle
- Respiratory variation in mitral and tricuspid flow
Cardiac MRI or CT Scan
- Offers more detailed imaging when an echocardiogram is inconclusive
Treatment of Cardiac Tamponade
The primary goal of treatment is to relieve pressure on the heart and address the underlying cause. Management strategies differ based on the severity and aetiology of tamponade.
Emergency Pericardiocentesis
- The most common and immediate treatment
- A needle is inserted into the pericardial space to aspirate fluid
- Guided by echocardiography or fluoroscopy
Surgical Pericardiotomy (Pericardial Window)
- Used for recurrent effusions or when pericardiocentesis is ineffective
- Involves creating an opening in the pericardium to allow continuous drainage
Intrapericardial Therapy
- In cancer-related effusions, chemotherapy or sclerosing agents may be instilled into the pericardial space
Treatment of Underlying Causes
- Antibiotics for infections
- Anti-inflammatory agents for autoimmune conditions
- Dialysis for uremic pericarditis
- Oncologic therapy for malignancy-related effusion
Complications of Cardiac Tamponade
If not treated promptly, cardiac tamponade can lead to serious and even fatal complications:
- Cardiogenic shock
- Pulmonary edema
- Organ failure
- Cardiac arrest
Following successful treatment, patients may still require monitoring for:
- Recurrence of pericardial effusion
- Infection or bleeding at the pericardiocentesis site
- Constrictive pericarditis
Prognosis and Long-Term Outlook
The prognosis of cardiac tamponade depends largely on the speed of diagnosis, cause, and timeliness of treatment. When treated promptly, outcomes are generally favourable, particularly in traumatic or iatrogenic cases.
In contrast, tamponade related to malignancy or chronic kidney disease may recur or indicate poor prognosis due to the underlying condition.
Patients are advised to:
- Follow up regularly with their cardiologist
- Monitor for symptoms of recurrence
- Manage chronic conditions proactively
Living with Cardiac Tamponade: Recovery and Follow-Up
Recovering from cardiac tamponade involves both physical healing and ongoing medical monitoring. Here are some recommendations for patients post-treatment:
Short-Term Recovery
- Rest and avoid strenuous activity for 1–2 weeks post-procedure
- Monitor blood pressure and heart rate regularly
- Watch for signs of recurrence (e.g., chest pain, shortness of breath)
Long-Term Management
- Address and treat underlying conditions (e.g., cancer, autoimmune disease)
- Consider lifestyle changes to reduce cardiac strain: a low-sodium diet, moderate exercise
- Regular echocardiograms as advised
FAQs
Is Cardiac Tamponade the Same as Pericardial Effusion?
No. While tamponade is caused by a pericardial effusion, not all effusions cause tamponade. Tamponade is defined by hemodynamic compromise.
Can Cardiac Tamponade be Prevented?
Prevention depends on managing risk factors like kidney failure, cancer, and avoiding complications from invasive procedures.
How Fast Can Cardiac Tamponade Become Fatal?
Very rapidly. Acute tamponade can cause cardiac arrest within minutes if not treated immediately.
Will Tamponade Recur After Treatment?
It depends on the underlying cause. Recurrent effusions are more common in malignancy or autoimmune conditions.
Conclusion
Cardiac tamponade is a critical condition that demands prompt recognition and skilled intervention. Although rare, it can occur in a wide range of clinical scenarios—from trauma to chronic diseases like cancer and kidney failure. At Harley Street Heart & Vascular Centre, we offer advanced diagnostic and therapeutic capabilities to manage cardiac tamponade with precision and care.
If you or a loved one experiences symptoms of cardiac distress, do not delay—contact our heart clinic or cardiologists for immediate evaluation and life-saving treatment.
Contact us for more information or to book an appointment.
This write-up has been medically reviewed by Dr. Michael Ross MacDonald, a consultant cardiologist at The Harley Street Heart & Vascular Centre in Singapore, to ensure the accuracy and reliability of the information provided