PERICARDITIS
Introduction to Pericarditis
What if you suddenly feel a sharp pain in your chest that worsens when you breathe in or lie down? What if you also experience shortness of breath, fever, and fatigue? These could be signs of pericarditis, an inflammation of the thin tissue that surrounds the heart (pericardium)
To learn more about it, scroll down or schedule an appointment with one of our cardiologists.
Definition and Overview
Pericarditis is inflammation of the pericardium that can manifest as intense and abrupt, lasting only a brief time, or as a long-term condition persisting for months or even years.
The exact cause is often unclear, however, it can arise from viruses, viral or bacterial infections, autoimmune diseases, heart damage, certain medications and unknown causes (idiopathic pericarditis).
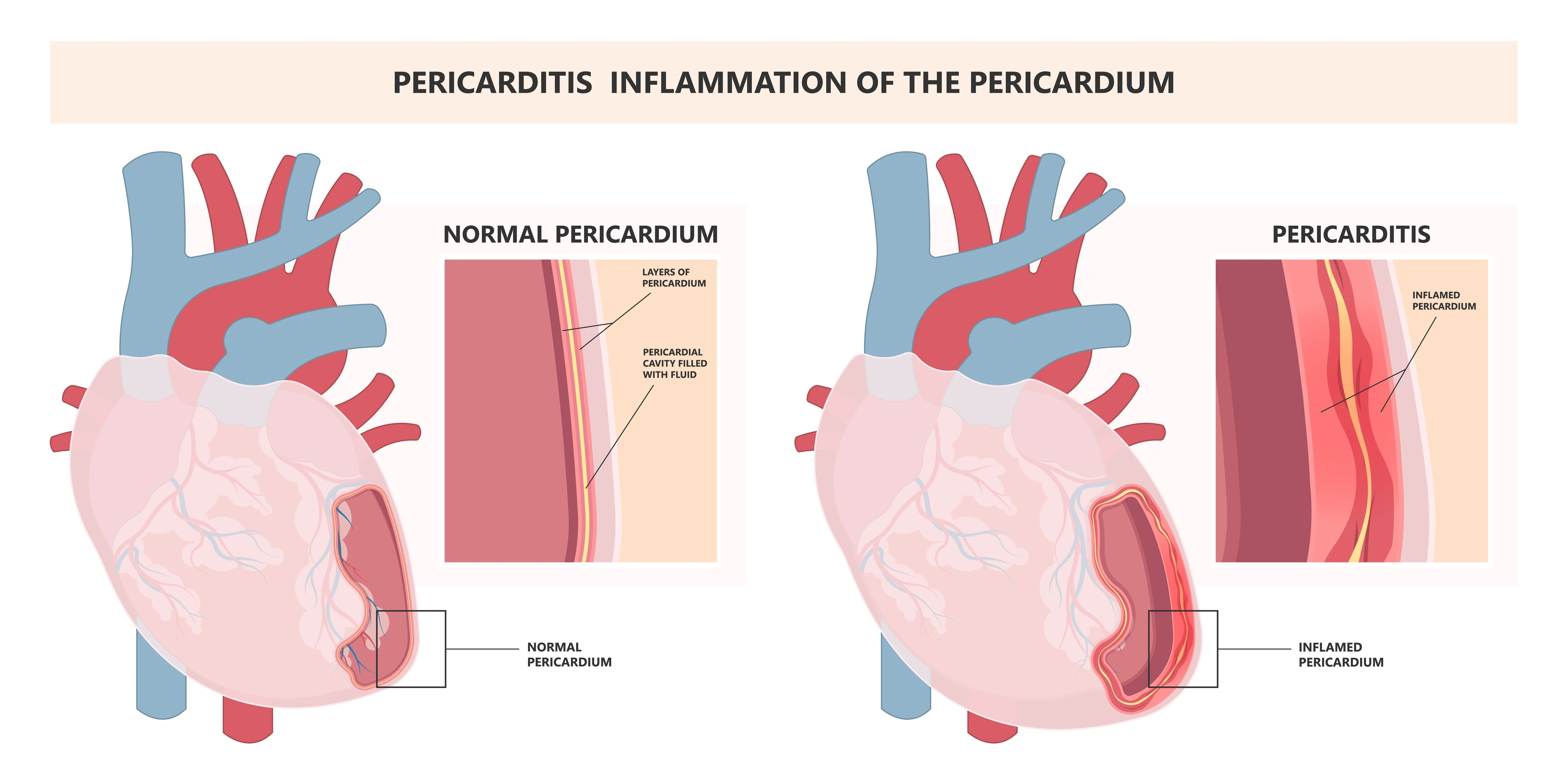
Importance of the Pericardium
The pericardium does several important jobs, such as protecting your heart from physical trauma, keeping your heart in place, lubricating your heart, and preventing infection.
The pericardium is also important for normal heart function. It helps to maintain the correct pressure around the heart and prevents it from collapsing. Additionally, it helps to distribute electrical impulses throughout the heart, which is essential for normal heart rhythm.
Types of Pericarditis
There are several types of pericarditis, each with its unique characteristics. They are acute pericarditis, chronic pericarditis, and recurrent pericarditis. Understanding the different types can help your doctor diagnose your condition and recommend the best course of treatment.
Acute Pericarditis
Often characterised by chest pain that gets worse with deep breaths or lying down, this type develops suddenly and lasts for less than 6 weeks. It is the most common type and is often caused by a viral infection.
Causes and Risk Factors
Acute pericarditis may be caused by a variety of factors, such as bacterial infections, autoimmune diseases, such as lupus, cancer, heart attack, heart surgery, chest trauma and medications. The risk factors include age and sex. Moreover, it is most common in people between the ages of 20 and 50 and men as compared to women.
Symptoms
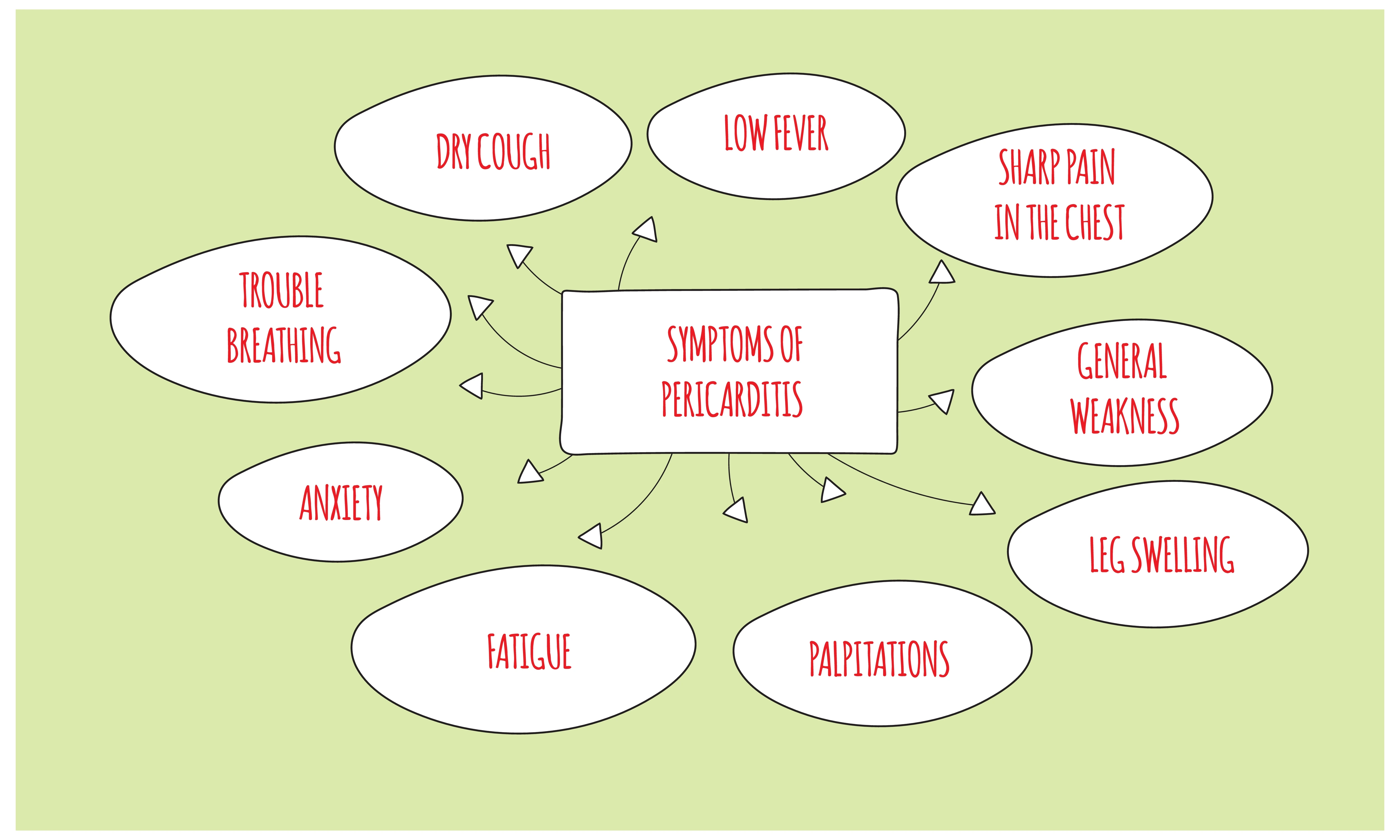
Symptoms of acute pericarditis are sharp, stabbing chest pain. The pain is often worse when you lie down or take a deep breath. It may also radiate to your neck, shoulder, or back. Other symptoms may include shortness of breath, fatigue, cough, fever, palpitations, anxiety, and leg swelling.
Diagnosis
To diagnose acute and recurrent pericarditis, your doctor will ask you about your symptoms and medical history. They will also perform a physical exam and listen to your heart with a stethoscope.
If your doctor suspects that you may have it, they may order some tests to help confirm the diagnosis, such as chest X-ray, electrocardiogram (EKG), echocardiogram and blood tests.
Chronic Pericarditis
Chronic pericarditis lasts for more than three months. While it is rare, it can be serious and lead to complications such as constrictive pericarditis and cardiac tamponade.
Causes and Risk Factors
The causes of chronic pericarditis are not fully understood, this rare condition is thought to be caused by a combination of genetic and environmental factors such as autoimmune diseases, cancer, heart surgery, radiation therapy, certain antibiotics and cancer drugs.
Symptoms
The most common symptoms of chronic pericarditis are sharp chest pain, shortness of breath, fatigue, fever, cough, heart palpitations and leg swelling.
Diagnosis
Your doctor will ask about your symptoms and medical history to diagnose chronic pericarditis. They may also order some tests, such as chest X-rays, electrocardiogram (EKG), echocardiogram, and blood tests to help confirm the diagnosis.
Recurrent Pericarditis
Recurrent pericarditis is a condition in which pericarditis returns after a symptom-free interval. It is a relatively common condition, affecting up to 30% of people who have had pericarditis in the past.
Characteristics
Recurrent pericarditis is a more complex form of pericarditis. Characterised by repeated episodes, this type of pericarditis occurs for at least 4 to 6 weeks after the previous episode has resolved
Management
The management of recurrent pericarditis is complex and should be individualised based on the patient's presentation and response to therapy. The goals of treatment are to reduce inflammation and relieve symptoms, prevent further episodes of pericarditis, and prevent complications, such as the risk of constrictive pericarditis and cardiac tamponade
Pericarditis Causes and Risk Factors
The cause of pericarditis is often associated with Infections, such as viral, bacterial, or fungal infections. It is also more commonly observed in males and individuals aged between 20 and 50. Understanding the causes and risk factors associated with pericarditis is crucial for proper diagnosis and treatment of this condition.
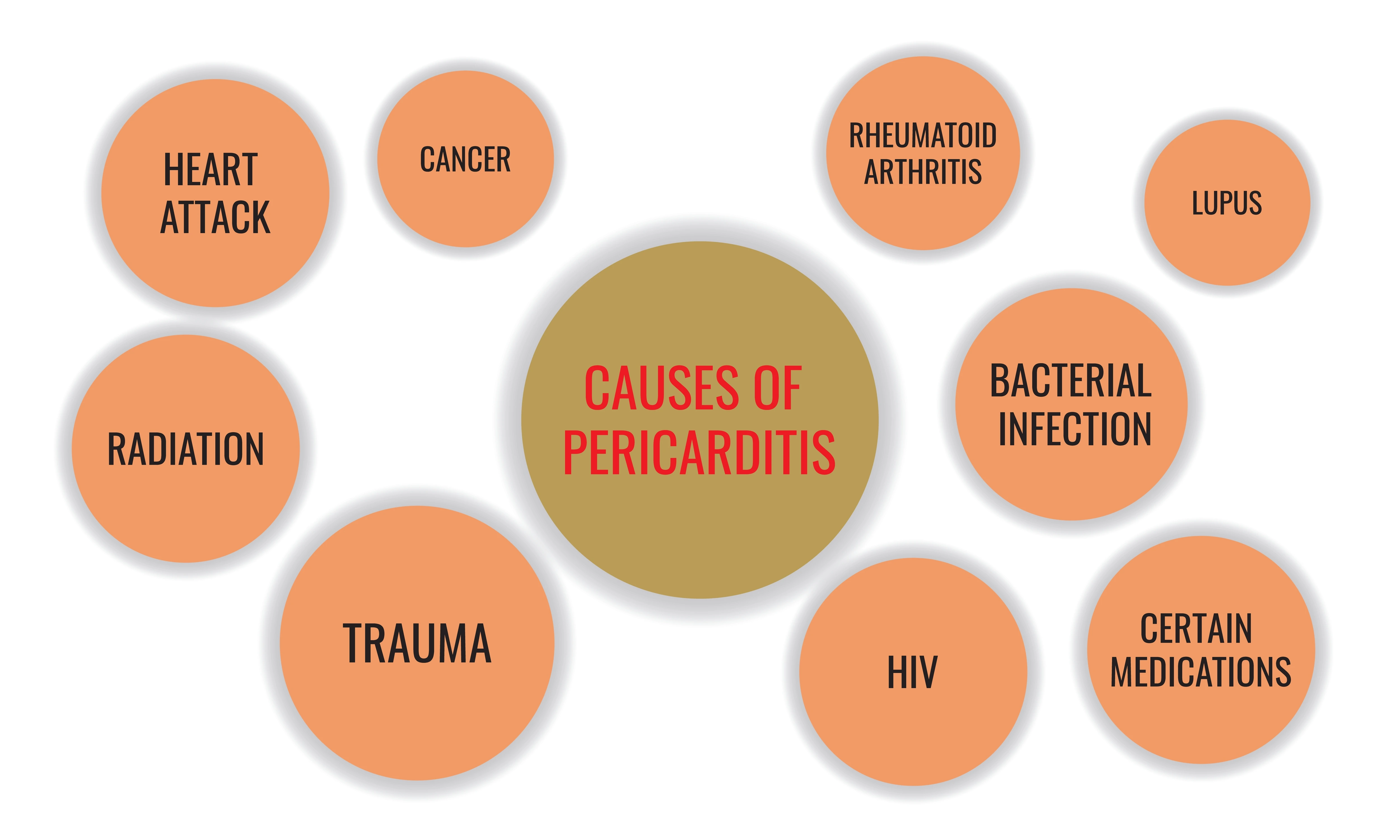
Infectious Causes
Infectious pericarditis is caused by an infection of the pericardium. It is the most common type of pericarditis, accounting for up to 90% of all cases.
Viral Infections
It is not fully understood how viral infections cause pericarditis. However, it is thought that the virus may directly infect the pericardium or trigger an autoimmune response that causes inflammation of the heart tissue.
Bacterial Infections
Bacterial pericarditis, though less common than viral pericarditis, poses a greater threat and demands swift treatment to avert potential life-threatening consequences. This form of pericarditis can manifest through various pathways. It may result from the spread of bacteria to the pericardium originating from a nearby infection like pneumonia or empyema, where pus accumulates between the lungs and chest wall. Alternatively, bacteria can be transported through the bloodstream from a distant infection, such as an infection of the heart's inner lining, chest trauma, as well as post-heart surgery.
Fungal Infections
Fungal pericarditis usually occurs from spores being inhaled, spreading from nearby infection, chest injury operation, heart surgery, or a fungal infection that has spread to multiple organs in the body.
Non-Infectious Causes
It is less common than infectious pericarditis, but it can be more difficult to treat. To diagnose it your doctor will ask you about your symptoms, and medical history. They can also suggest you do some tests such as blood tests, electrocardiogram (EKG), echocardiogram and check the fluid in the pericardium.
Autoimmune Conditions
Autoimmune diseases are one of the most common causes of non-infectious pericarditis. In autoimmune diseases, the body's immune system mistakenly attacks its tissues, causing inflammation.
Trauma or Injury
Pericarditis caused by trauma or injury is a rare but serious condition. It can occur after a chest injury, such as a blunt force injury from a car accident or fall, or a penetrating injury from a knife or gunshot wound.
The trauma to the chest can damage the tissue that surrounds the heart. This can lead to inflammation and swelling of the pericardium, which can put pressure on the heart and make it difficult to beat properly.
Medications
Certain medications have been linked to pericarditis or trigger an autoimmune response that causes inflammation of the pericardium. They are antibiotics, cancer drugs, anticoagulants, anticonvulsants, and nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen.
Radiation
Radiation therapy can harm the pericardium, the lining around your heart, directly or by causing the body's immune system to attack it.
Recognizing the Symptoms
Recognising the symptoms is crucial to prompt diagnosis and treatment. A healthcare professional will conduct a physical examination, review the patient's medical history and symptoms, and possibly perform additional tests to confirm the diagnosis and determine the best course of treatment.
Common Symptoms
Pericarditis symptoms may differ but commonly involve fatigue and chest discomfort that could intensify while taking deep breaths or when in a lying position. Some people might also have difficulty breathing or experience a raised body temperature.
Chest Pain
Chest pain, a common symptom in various medical conditions, can also arise from pericarditis. This condition can cause discomfort or a sharp, piercing pain in the chest that may worsen with deep inhalation or when lying flat. The symptoms of pericarditis are similar to heart attack, but there are some key differences. The chest pain associated with pericarditis is often sharp and stabbing, while the chest pain associated with a heart attack is often described as a crushing or squeezing sensation. The pain associated with pericarditis may radiate to the neck, shoulders, and back, while the pain associated with a heart attack is typically limited to the chest. Additionally, it may include shortness of breath, fatigue, cough, fever, palpitations, anxiety, and leg swelling, while these symptoms are less common with a heart attack.
Fever
Fever, a common symptom of various medical conditions, is the increase of body temperature above the normal range. It serves as an indicator of an underlying infection or inflammation within the body. A fever associated with pericarditis is typically mild and varies during the day. It is important to seek medical attention if one experiences persistent fever, as it could indicate a more serious condition and require emergency treatment.
Difficulty Breathing
In the context of pericarditis, shortness of breath can be a distressing symptom experienced by individuals. This condition can result in the build-up of fluid buildup around the heart, which compresses the heart. The limited movement and impaired filling of the heart can lead to reduced oxygen supply to the body, leading to shortness of breath. Additionally, the inflammation itself can irritate the breathing muscle, affecting its function and worsening breathing difficulties.
Fatigue
Fatigue along with chest pain, fever, and shortness of breath, is one of the prominent symptoms of pericarditis. The exact mechanism behind the fatigue experienced in pericarditis is not fully understood. However, it is believed to be multifactorial, including factors such as the body's immune response to inflammation and the increased energy demands due to the underlying illness. Managing pericarditis and alleviating fatigue may involve the use of anti-inflammatory medications, rest, and proper medical care to address the underlying cause.
Atypical Symptoms
Atypical symptoms of pericarditis can confuse both patients and healthcare providers. Typically, characterised by chest pain, abdominal pain, shoulder pain and pericardial friction rub. These symptoms may vary in intensity and duration, making diagnosis challenging.
When atypical symptoms are present, further evaluation and diagnostic tests, such as echocardiograms or cardiac MRI, may be necessary to confirm the diagnosis and rule out other potential cardiac issues.
Abdominal Pain
Abdominal pain refers to a sensation of discomfort or distress in the area between the chest and the pelvis. It can be acute or chronic and encompasses a wide range of potential causes. Although pericarditis primarily affects the heart and can cause chest pain, it can occasionally radiate to the abdomen, leading to abdominal pain.
Shoulder Pain
While the main symptom of pericarditis is chest pain, it can also result in pain radiating to the shoulder and neck. This can be a sharp or dull pain and may worsen with certain movements or deep breaths.
Pericardial Friction Rub
When inflamed, the pericardial layers rub against each other and may produce a grating or squeaking sound. This sound is typically heard with a stethoscope and can be described as similar to the sound of rubbing sandpaper.
Diagnosing Pericarditis
The diagnosis is typically made through a combination of medical history, physical examination, and diagnostic tests. Once diagnosed, the prognosis of pericarditis depends on various factors, including the underlying cause, the extent of inflammation, and the promptness of treatment.
Physical Examination
A physical assessment plays a key role in identifying particular indications of pericarditis, such as discomfort in the chest, irregular heart sounds, and the presence of a pericardial friction rub.
Listening for Pericardial Friction Rub
Listening for a pericardial friction rub is an important component of a physical examination when evaluating for pericarditis. The inflammation can cause the pericardial layers to rub against each other, producing a characteristic sound known as a friction rub. The examiner listens for a high-pitched scratching or grating sound that is synchronous with the heartbeat. This sound is best heard when the patient is sitting up and leaning forward.
Assessing Vital Signs
Assessing vital signs involves the measurement of key indicators such as body temperature, heart rate, respiratory rate, and blood pressure. These measurements provide information on an individual's physiological functioning and can indicate the presence of underlying health conditions. For example an increased heart rate and fever.
Diagnostic Tests
When evaluating a patient with suspected pericarditis, several diagnostic tests are commonly employed. The accurate and timely utilisation of these diagnostic tests aids in the effective management of pericarditis and improves patient outcomes.
Electrocardiogram (ECG)
An electrocardiogram (ECG) is a diagnostic tool used to measure the electrical activity of the heart. The ECG provides valuable information about the heart's rhythm, rate, and overall function, allowing doctors to identify any abnormalities that may be present. By analysing the ECG, healthcare professionals can identify characteristic changes indicating pericarditis, such as ST segment elevations or depressions, helping in the accurate diagnosis and subsequent treatment of the condition.
Echocardiogram
An echocardiogram will help cardiology doctors to assess the size, structure, and function of the heart. By examining the images obtained from an echocardiogram, doctors can detect any abnormalities or signs of pericarditis and provide appropriate treatment for the patient.
Blood Tests
A blood test can spot specific blood markers that indicate inflammation in the body and can help confirm the diagnosis. Additionally, blood tests can also be used to identify potential underlying causes of pericarditis, such as viral or bacterial infections. Regular blood tests may be required to monitor the progress of treatment and ensure the inflammation is subsiding.
Chest X-ray
A chest X-ray can help identify any abnormal heart size, shape, or position of the heart and is one of the important tools in assessing the extent of pericarditis.
Cardiac MRI
Cardiac MRI is particularly useful in evaluating pericarditis. By visualising the pericardium, cardiologists can identify signs of inflammation, such as fluid accumulation or thickening, aiding in the accurate diagnosis of pericarditis. Additionally, this imaging technique can guide determining the extent of pericardial involvement and monitoring the effectiveness of treatment strategies for pericarditis.
Pericarditis Treatment and Management
Pericarditis is treated through a combination of treatments and a well-defined recovery timeframe. By implementing timely therapy, such as anti-inflammatory medications, physicians can alleviate the symptoms and reduce the risk of complications. Additionally, rest and lifestyle modifications are crucial during the recovery phase.
Treating the Underlying Cause
To effectively treat pericarditis, it is essential to identify and address the root cause. This means identifying and treating the underlying condition that is causing the pericarditis.
Managing Symptoms
Managing symptoms of pericarditis involves a combination of medication and lifestyle changes. Medications are commonly prescribed to reduce inflammation, manage pain and reduce inflammation. Lifestyle changes such as reducing physical activity and managing stress can also help manage symptoms. Additionally, adopting a healthy lifestyle by eating a balanced diet, exercising regularly, and getting enough sleep can contribute to overall well-being and symptom management.
Pain Relief (NSAIDs)
Nonsteroidal anti-inflammatory drugs (NSAIDs) are a class of medications commonly used to relieve pain and inflammation. By reducing inflammation, NSAIDs help alleviate symptoms like chest pain and fever associated with pericarditis. However, it is important to use NSAIDs cautiously as they can have side effects such as gastrointestinal bleeding and increased risk of cardiovascular events.
Colchicine
Colchicine is a medication that has been used for centuries in the treatment of gout. However, its versatility extends beyond gout, as it helps prevent white blood cells from moving to the inflamed area and further worsen tissue inflammation.
Imagine the pericardium as a balloon around the heart that becomes inflamed and swollen. This can make it difficult for the heart to expand and contract properly as if the balloon is too tight. Colchicine can help to reduce the inflammation and swelling of the pericardium, making it easier for the heart to beat.
Corticosteroids
Corticosteroids are a class of medications that are like the body's own stress hormone, cortisol. They are powerful anti-inflammatory drugs that can be used to treat a variety of conditions, including pericarditis.
Corticosteroids work by reducing inflammation and suppressing the immune system. This can help to relieve the symptoms of pericarditis quickly and effectively.
Lifestyle Modifications
Lifestyle modifications are often recommended as part of the treatment plan for pericarditis. Regular exercise is beneficial for improving cardiovascular health and reducing the risk of complications, but individuals with pericarditis may need to modify their exercise regimen to avoid triggering symptoms.
Lifestyle modifications are often recommended as part of the treatment plan for pericarditis. Individuals with pericarditis may need to modify their exercise regimen to avoid triggering symptoms.
Rest and Activity Level
It is important to avoid activities that may strain the heart and instead focus on low-impact exercises such as walking or swimming. It is important to avoid activities that may strain the heart and instead focus on low-impact exercises to lower the risk of future flare-ups.
Diet and Fluid Intake
Diet and fluid intake play important roles in maintaining overall health as certain dietary factors can increase the risk of developing pericarditis. It is crucial to limit the consumption of processed foods, saturated fats, and salt, as they can lead to inflammation and fluid retention in the body. On the other hand, incorporating a balanced and nutritious diet with fruits, vegetables, whole grains, lean proteins, and healthy fats can help reduce inflammation and promote heart health. Furthermore, staying hydrated by drinking an adequate amount of water throughout the day is essential for maintaining proper fluid balance in the body and preventing dehydration, which can strain the heart.
Stress Management
Excessive stress can have detrimental effects on both physical and mental health. While pericarditis can also be caused by other factors, high levels of stress have been linked to increased susceptibility. Therefore, implementing stress management techniques can help reduce the risk of developing pericarditis. Techniques such as deep breathing exercises, regular physical activity, mindful meditation, and engaging in hobbies can effectively alleviate stress.
Complications and Long-Term Outlook
While most cases of pericarditis are acute and resolve within a few weeks, some individuals may experience complications and require long-term management. One potential complication of pericarditis is the development of pericardial effusion, which occurs when fluid accumulates within the pericardium. In severe cases, this can lead to cardiac tamponade, a life-threatening condition requiring immediate medical intervention.
The long-term outlook for individuals with pericarditis depends on various factors such as the underlying cause, the presence of complications, and the response to treatments. Regular monitoring, lifestyle modifications, and appropriate management can help optimise outcomes and improve the quality of life for those affected by pericarditis.
Potential Complications
Potential complications of pericarditis can range from mild to severe. In some cases, pericarditis can lead to the accumulation of fluid around the heart, compression by fluid and recurrence. Early diagnosis and treatment are crucial in preventing these complications and ensuring the best possible outcomes for individuals with pericarditis.
Pericardial Effusion
The accumulation of fluid in the layers of the pericardium is called a pericardial effusion. As the fluid builds up in the pericardium, it puts pressure on the heart, impacting its ability to pump blood efficiently. Immediate medical attention is necessary to diagnose and treat pericardial effusion to prevent life-threatening complications.
Cardiac Tamponade
Cardiac tamponade is a life-threatening condition that occurs when fluid accumulates in the pericardial space, putting pressure on the heart and impairing its ability to pump blood effectively. The treatment for cardiac tamponade typically involves draining the excess fluid from the pericardial space and avoiding its potentially life-threatening consequences.
Recurrence
While treatment for pericarditis can alleviate symptoms and promote healing, there is a risk of recurrence in some cases. Factors like underlying medical conditions or infections can contribute to the recurrence of pericarditis.
Long-Term Prognosis
The long-term prognosis of pericarditis is generally good. If the underlying cause of pericarditis is identified and treated effectively, most individuals will recover fully without complications. However, in some cases, pericarditis can become chronic and recur frequently, leading to a more challenging prognosis.
Recurrence Risk
Recurrent episodes of pericarditis can cause scarring and thickening of the pericardium, which may impair its function. This can result in complications such as constrictive pericarditis, which can lead to heart failure. Additionally, some individuals may develop complications like pericardial effusion, where fluid accumulates around the heart, requiring further intervention.
Monitoring and Follow-up
Regular follow-up with a healthcare professional and adherence to prescribed treatments can help manage pericarditis and improve the long-term prognosis for individuals affected by this condition.
Prevention
Prevention is key! Preventive measures include managing viral and bacterial infections promptly and effectively, vaccinations, lifestyle changes and managing underlying conditions.
Prevention Strategies
Prevention strategies play a crucial role in minimising the risk of pericarditis. Several key measures can help prevent this condition and its potential complications.
Vaccinations
Vaccinations are a crucial aspect of public health, protecting against several infectious diseases. They work by introducing a weakened or inactive form of a pathogen into the body, stimulating the immune system to produce antibodies that recognise and destroy the pathogen that might contribute to the development of pericarditis.
Lifestyle Changes
First and foremost, maintaining good overall health by leading a healthy lifestyle is essential. This includes adopting a well-balanced diet, engaging in regular physical activity, and managing stress effectively. Additionally, practising good hygiene and avoiding exposure to respiratory infections can help prevent pericarditis caused by viral or bacterial infections.
Managing Underlying Conditions
It is also important to promptly treat any underlying conditions that increase the risk of pericarditis, such as autoimmune diseases or heart attacks. By actively managing underlying conditions, you can minimise the probability of the disease worsening or coming back.
Conclusion
Pericarditis can be a scary and confusing condition, but you don't have to go through it alone. At The Harley Street Heart and Vascular Centre, we'll provide you with personalized support and guidance throughout your treatment. We understand that every patient is different, so we'll work with you to develop a treatment plan that's right for you. Book an appointment or teleconsultation with us today, and let us help you get back to living your life to the fullest.
Frequently Asked Questions About Pericarditis
What Are the Symptoms of Pericarditis Pain?
The most common symptom of pericarditis is chest pain, which can range from mild discomfort to severe, sharp pain. This pain is typically located in the centre or left side of the chest and may radiate to the neck, shoulders, or back. It is often worsened by deep breathing, coughing, or lying flat on the back. Other symptoms may include a low-grade fever, fatigue, shortness of breath, and a dry cough.
Is Pericarditis Life-Threatening?
While pericarditis can be uncomfortable, it is typically not life-threatening. Most cases of pericarditis are acute and resolve on their own with rest and supportive care. However, in some instances, pericarditis can lead to complications that can be more serious. These complications may include pericardial effusion, fluid accumulation and where the pericardium becomes thickened and rigid, affecting the heart's ability to pump blood effectively.
What Is the Main Cause of Pericarditis?
The most common causes of pericarditis include a viral infection, specifically a viral infection of the respiratory tract such as influenza known to trigger pericarditis. Other potential causes include bacterial and fungal infections, as well as autoimmune disorders.
How Serious Is Pericarditis?
In most cases, pericarditis is not considered a serious condition and can resolve on its own with rest and medication. However, some cases can be more severe and may require medical intervention.
What Does the Start of Pericarditis Feel Like?
Pericarditis typically presents as sharp, stabbing chest pain that worsens with deep breathing, coughing, or lying down. The pain associated with pericarditis is often felt in the centre or left side of the chest and may radiate to the neck, back, or left shoulder.
Is Pericarditis Life-Threatening?
While pericarditis can be a painful and uncomfortable condition, it is generally not life-threatening. However, in some cases, complications can arise that may pose a risk to the individual's life. One potential complication is the accumulation of fluid in the pericardial sac which can put pressure on the heart and interfere with its ability to function properly.
What Is the Life Expectancy of Someone With Pericarditis?
The life expectancy of someone with pericarditis primarily depends on the severity and complications associated with the condition. With prompt diagnosis and treatment, most people make a full recovery without any complications. However, in some cases, it can lead to complications, such as constrictive pericarditis and cardiac tamponade, which can reduce life expectancy.
Can You Have Pericarditis and Myocarditis?
Yes, it is possible to have both at the same time as they are two separate conditions that affect different parts of the heart. Pericarditis refers to the inflammation of the thin tissue that surrounds and protects the heart. On the other hand, myocarditis is the inflammation of the heart muscle.


