ANGINA

Angina: Symptoms, Risk Factors, and Treatment

Angina is a type of pain in the chest that occurs when there is reduced blood flow to the heart muscle. It's often described as feeling like a squeezing or pressure in the chest. Angina is usually not life-threatening, but it is a symptom of an underlying heart problem, such as coronary artery disease. The most common cause of angina is coronary artery disease, a condition where the arteries that supply blood to the heart become narrowed or blocked due to the buildup of plaque.
What Is Angina?
Defining Angina
Angina, also known as angina pectoris or ischemic chest pain, occurs when the heart muscle doesn't receive enough oxygen-rich blood. Therefore, in angina episodes, the heart may beat faster and harder to gain more blood. It's a warning sign that there may be a problem with the blood flow to your heart, which can also increase the risk of a heart attack.
Angina Pectoris Symptoms
The most common symptom of angina is chest pain or discomfort. The pain of angina can feel like a squeezing, pressure, heaviness, tightness, or pain in your chest. Usually, the pain lasts for more than 10 minutes and may also radiate to your arms, shoulders, neck, jaw, or back.
Chest Pain or Discomfort
Angina is rare and typically caused by the narrowing of the coronary arteries, which reduces blood flow to the heart. When the heart muscle doesn't receive enough blood, it can lead to chest pain or discomfort.
Causes of Angina
The primary cause of angina is reduced blood flow to the heart. This can be due to various factors, including coronary artery disease, high blood pressure, or a spasm of the coronary arteries.
Risk Factors for Angina
Several risk factors can increase the likelihood of developing angina, including high blood pressure, smoking, high cholesterol, diabetes, lack of physical activity, and a family history of heart disease.
Types of Angina
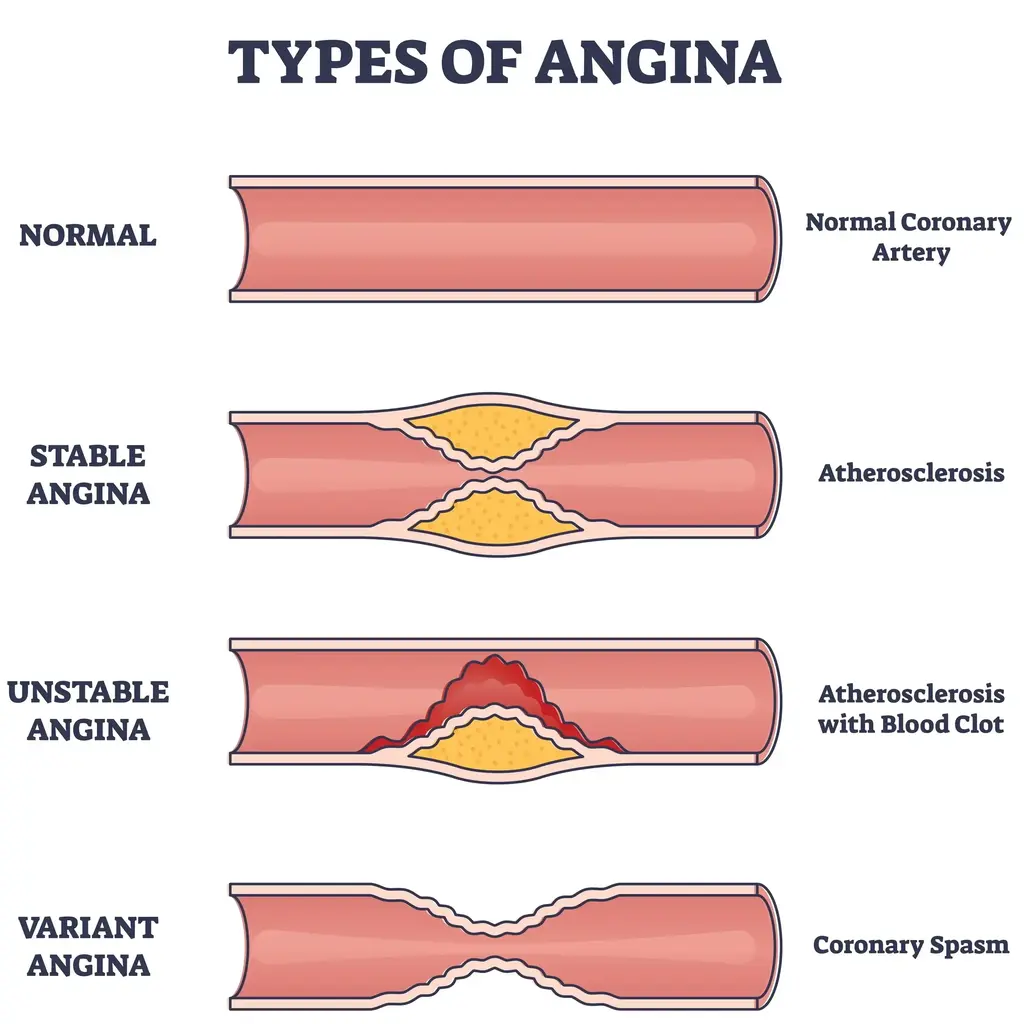
Stable Angina
Stable angina is the most common type of angina. The symptoms of stable angina are predictable and usually occur with physical activity, emotional stress, or cold weather. The pain is often relieved by rest or medication.
Symptoms of Stable Angina
Common symptoms of stable angina include chest pain, pressure, heaviness, tightness, or squeezing in the chest that may spread to the arms, shoulders, neck, or jaw.
Causes of Stable Angina
The leading cause of stable angina is the narrowing of the coronary arteries, which limits blood flow to the heart muscle. This narrowing is typically caused by a build-up of plaque (atherosclerosis) on the artery walls. When the heart muscle doesn't receive enough blood and oxygen, it can cause chest pain or discomfort.
Unstable Angina
Unstable angina is a more severe and unpredictable type of angina. The symptoms of unstable angina can occur at rest and may not be relieved by medication or rest. It is considered a medical emergency.
Symptoms of Unstable Angina
Unstable angina is characterised by sudden and unexpected chest pain or discomfort that may be more severe and last longer than stable angina. It can last longer than 15 to 20 minutes.
Causes of Unstable Angina
Unstable angina happens for reasons similar to stable angina, where blood clots partially or fully block an artery. But unlike stable angina, unstable angina is more severe and unpredictable, signalling a potentially critical blockage in the heart's arteries.
Microvascular Angina
Microvascular angina, also known as cardiac syndrome X, is a type of angina that affects the small coronary arteries (less than a millimetre across). Microvascular angina is more common in women, particularly those who are postmenopausal. Additionally, it is also common in individuals with diabetes, hypertension, or a smoking habit.
Symptoms of Microvascular Angina
The symptoms of microvascular angina are similar to those of stable angina but may occur with less physical exertion or emotional stress.
Causes of Microvascular Angina
The exact cause of microvascular angina is not fully understood, but it is believed to be related to abnormalities in the small blood vessels of the heart that do not widen the way they should. Spasms in the blood vessels may also cause it.
Prinzmetal's Angina
Prinzmetal's angina or variant angina is a rare form of angina caused by a spasm in the coronary arteries, leading to a temporary reduction in blood flow to the heart.
Symptoms of Prinzmetal's Angina
Prinzmetal's angina is characterised by episodes of chest pain that often occur at rest and may be more severe than other types of angina.
Causes of Prinzmetal's Angina
The exact cause of Prinzmetal's angina is unknown, but it is thought to be related to spasms in the coronary arteries, genetics, and blood vessel abnormalities.
Angina in Women
Women may experience angina symptoms differently than men. Women are more likely to have microvascular angina and may present with atypical symptoms such as fatigue, shortness of breath, nausea, or stabbing pain.
Diagnosis and Treatment
Diagnosing Angina
Diagnosing angina involves a thorough medical history, physical examination, and tests such as electrocardiogram, stress test, echocardiogram, coronary angiography, or cardiac CT scan to determine the extent and severity of the condition.
Treatment Options
The goal is to relieve symptoms, prevent complications, and improve overall heart health. Treatment of angina may include lifestyle changes, medication, angioplasty, stenting, or coronary artery bypass grafting.
Angina Medication
Medications commonly prescribed for angina include nitroglycerin, beta-blockers, calcium channel blockers, and antiplatelet drugs to reduce chest pain and improve blood flow to the heart.
Preventing Angina
Preventing angina involves managing risk factors such as high blood pressure, high cholesterol, diabetes, and obesity through lifestyle modifications, including a heart-healthy diet, regular exercise, and smoking cessation.
Managing Angina Risk
Other strategies for managing angina risk include stress management, regular medical check-ups, and adherence to prescribed medications and lifestyle changes.
Living with Angina

Angina Lifestyle Management
People who are diagnosed with angina need to adopt a heart-healthy lifestyle, including a balanced diet, regular physical activity, stress reduction, and adherence to prescribed medications.
Recognising Warning Signs
Individuals with angina must recognise and seek immediate medical attention for warning signs of a heart attack, such as severe chest pain, shortness of breath, dizziness, or nausea.
Angina and Heart Attacks
While angina can be a sign of heart disease, it does not necessarily indicate a heart attack. However, people with angina have an increased risk of experiencing a heart attack or stroke.
Triggering Factors
Identifying and avoiding triggering factors such as physical exertion, emotional stress, extreme temperatures, or heavy meals can help manage angina symptoms and reduce the risk of angina attacks.
Adapting to Life with Angina
Adapting to life with angina may require making lifestyle adjustments and learning how to manage symptoms effectively to maintain a good quality of life. This may include regular follow-up appointments, cardiac rehabilitation programs, and education on heart-healthy habits.
Diet For Angina
A heart-healthy diet for angina includes consuming various fruits, vegetables, whole grains, lean proteins, and healthy fats while limiting sodium, saturated fats, and added sugars. Additionally, staying hydrated, managing portion sizes, and being mindful of alcohol consumption are also important.
Exercises For Angina
Regular physical activity, including aerobic exercises and strength training, can help improve cardiovascular health and reduce angina symptoms. Additionally, you must consult with your healthcare provider to create a safe and effective exercise plan that meets their specific needs and limitations.
Angina and Heart Health
Impact on Heart Health
Angina can have a significant impact on heart health, leading to complications such as heart attacks, arrhythmias, heart failure, or even sudden cardiac arrest if left untreated.
Angina and Other Heart Conditions
Individuals with angina may have an increased risk of developing other heart conditions, including coronary artery disease, heart failure, or hypertension.
Supporting Heart Function
Supporting heart function involves maintaining a healthy lifestyle, managing risk factors, adhering to prescribed medications, and seeking regular medical care to ensure optimal heart health.
Preventive Measures
Preventive measures for angina include regular medical check-ups, monitoring of blood pressure and cholesterol levels, and early intervention to address any signs of heart disease. Regular exercise, maintaining a healthy weight, and eating healthy food can also help prevent angina.
Recognising Symptoms
Individuals with angina need to recognise any changes in their symptoms and seek prompt medical attention if they experience new or worsening chest pain, shortness of breath, or dizziness.
Conclusion
Angina is a serious condition that requires careful management to reduce symptoms and prevent complications. By understanding the symptoms, risk factors, and treatment options for angina, individuals can take proactive steps to improve their heart health and overall well-being.
Frequently Asked Questions About Angina
Below are frequently asked questions about angina, its symptoms, causes, and treatments.
What Are the Symptoms of Angina?
The symptoms of angina usually include squeezing in your chest, pain and discomfort that can spread to the neck, jaw, arms, shoulders, or back. It can also cause a feeling of fullness or a choking sensation.
What Causes Angina?
Angina is typically caused by reduced blood flow to the heart muscles. This can happen when the coronary arteries narrow due to plaque buildup, reducing blood flow to the heart.
What Are the Treatments for Angina?
Treatment for angina may include medications such as aspirin, nitroglycerin, or beta-blockers, as well as lifestyle changes like a heart-healthy diet, regular exercise, and stress management. In some cases, surgery or other procedures may be recommended.
How Is Angina Diagnosed?
Angina is often diagnosed based on a person's medical history, symptoms, and diagnostic tests such as an electrocardiogram (ECG), stress test, coronary angiography, or cardiac CT scan.
What Are the Symptoms and Causes of Angina?
The symptoms and causes of angina are related to chest pain caused by reduced blood flow to the heart. Angina pain is often described as a squeezing or pressure in the chest, typically triggered by physical activity or emotional stress.
How Is Angina Different From a Heart Attack?
Angina is a symptom of underlying heart disease and is usually relieved by rest or medication. A heart attack, on the other hand, is caused by a complete blockage of blood flow to the heart and can cause permanent damage to the heart muscles if not treated promptly.
Can Angina Be a Sign of a Heart Attack?
Yes, angina can be a warning sign of a potential heart attack, especially if the symptoms become more frequent and severe or occur at rest. You must seek medical attention if you experience worsening or new symptoms.
How Can Angina Be Managed?
Angina can be managed by taking prescribed medications, making lifestyle changes, recognising and avoiding triggers, and attending regular medical check-ups to monitor and control the condition.
Are There Different Types of Angina?
Yes, there are different types of angina, including stable angina, unstable angina, variant (vasospastic) angina, and microvascular angina. Each type has distinct characteristics and may require different treatment approaches.
How Can Angina Be Prevented?
To help prevent and control angina, it's crucial to adopt a heart-healthy lifestyle, manage risk factors such as high blood pressure, high cholesterol, and diabetes, follow a prescribed treatment plan, and seek regular medical care to monitor and manage the condition.


