MEDBULLETIN SEPTEMBER 2020
Quiz
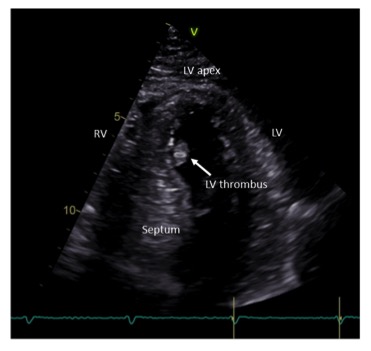
A 47-year-old man, who was previously fit and well, developed a non – ST elevation myocardial infarction whilst skiing in the USA earlier this year which was treated with percutaneous coronary intervention. He came to see me one week later after he returned to Singapore and felt well with no chest pain or breathlessness. His ECG (Figure A) and 4-chamber view of his echocardiogram (Figure B) when seen in clinic are shown below. His left ventricular (LV) ejection fraction measured 47% with anteroseptal regional wall motion abnormalities. What does the ECG and echo image show? How would you manage his condition?
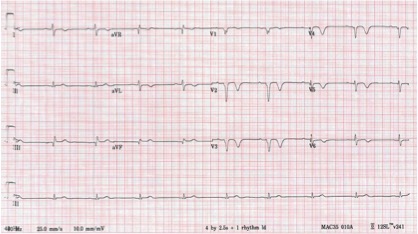
Fig A
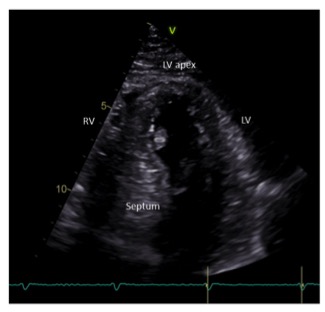
Fig B
Answer:
The ECG shows loss of anterior R waves, anterior Q waves and deep T wave inversion- all late ECG changes following an acute anterior myocardial infarction. The echocardiogram shows a reduced ejection fraction of 47% (normal is > 55%) as a result of the myocardial infarction and the presence of a LV thrombus attached to the anteroseptal wall.
This is likely fresh thrombus following the acute myocardial infarction and reduced contractility in the anteroseptal wall. The patient is at risk of embolization of the thrombus and requires full anticoagulation for six months to dissolve the thrombus. A repeat echocardiogram after 3 months showed that the LV thrombus had resolved (although the patient completed the full 6 months course of oral anticoagulation). The patient was treated with warfarin (target INR 2.0-3.0); there is some evidence that direct oral anticoagulants may also be effective at dissolving LV thrombus.
ANSWERS TO ECG QUIZ
MedBulletin April 2024
MedBulletin Dec 2023
MedBulletin May 2023
MedBulletin Nov 2022
MedBulletin May 2022
MedBulletin Nov 2021
MedBulletin Mar 2021
MedBulletin Sep 2020
MedBulletin April 2020
MedBulletin Sep 2019
MedBulletin March 2019
MedBulletin Sep 2018
MedBulletin March 2018
MedBulletin Sep 2017
MedBulletin March 2017
MedBulletin Sep 2016
2016 Quiz
2015 Quiz
MedBulletin April 2024
MedBulletin Dec 2023
MedBulletin May 2023
MedBulletin Nov 2022
MedBulletin May 2022
MedBulletin Nov 2021
MedBulletin Mar 2021
MedBulletin Sep 2020
MedBulletin April 2020
MedBulletin Sep 2019
MedBulletin March 2019
MedBulletin Sep 2018
MedBulletin March 2018
MedBulletin Sep 2017
MedBulletin March 2017
MedBulletin Sep 2016
2016 Quiz
2015 Quiz